How Gaming Vaccination Statistics Can Lead to Future Lockdowns
Expert decisions affect the efficacy of vaccines far more than is currently discussed. Instead of expert decision makers blaming antivaxers, they must take responsibility of their own decisions to avert future lockdowns.

As my historical posts on this blog will attest, I am profoundly optimistic about the ability of science to ultimately handle COVID-19. This is a point that has been proven through advances in treatment and vaccination.
Nevertheless, despite progress, parts of the world may find themselves returning to lockdown despite vaccination. Even more perversely, blame for this phenomena may be directed at ordinary citizens instead of Government officials.
For the purposes of this article, I'll be using the United States and United Kingdom as examples; but much of this is applicable to many countries around the world.
Recent news articles have pointed to how a surge of COVID-19 has driven ICU occupancy in Texas to 90%. This seems particularly alarming given the high coverage of vaccination in the United States.
Twitter experts will be quick to blame this on vaccine uptake caused by hesitant members of the population, but this is a naive understanding of the situation.
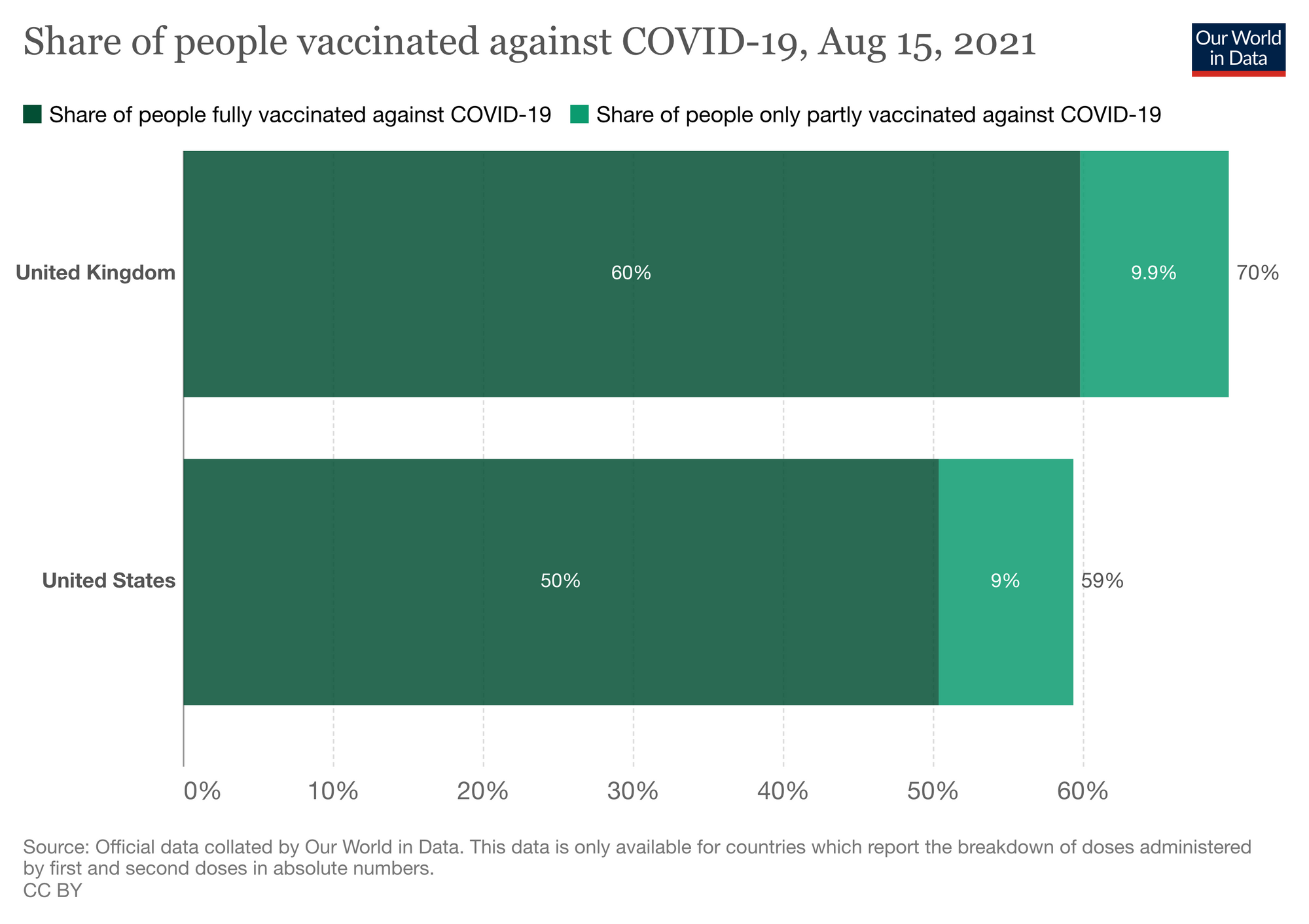
Indeed, there is only a 10-11% gap in vaccine rollout progress between the United States and the United Kingdom, and when the UK reached 0 COVID deaths for the first time, it was when vaccine coverage was lower than what the US currently has.
The vaccines used in both countries are largely comparable - both use mRNA vaccines (Pfizer/BioNTech and Moderna) alongside an adenovirus option (Oxford/Astrazeneca in the UK and Janssen in the US). Indeed, the US have more rapidly adopted novel mRNA vaccine technology, whilst the more tested Oxford/Astrazeneca vaccine did the bulk of the UK's early heavy lifting.
So why does there remain this apparent gap in COVID fatalities?
Strict Age Prioritisation
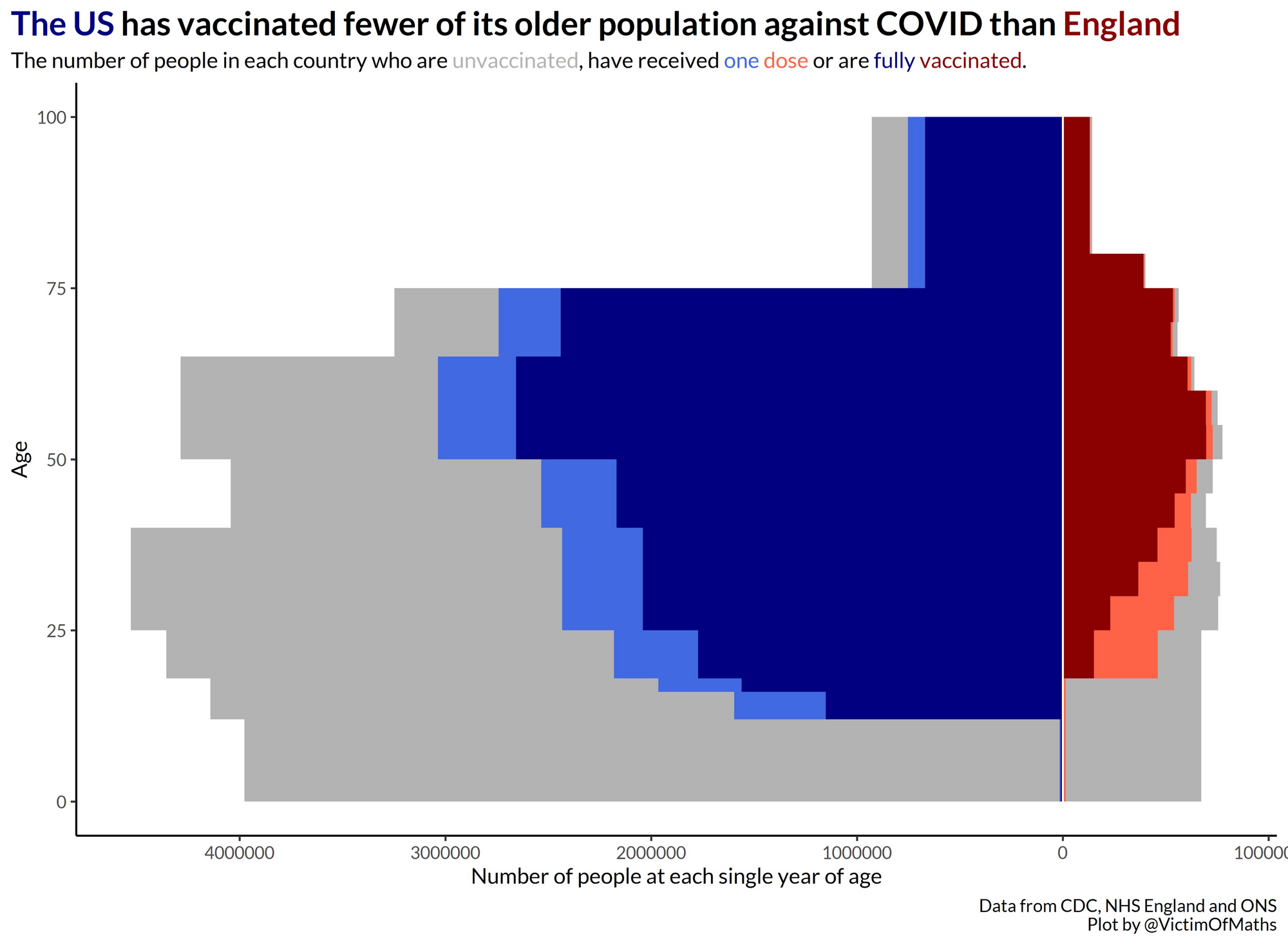
The UK adopted a strict approach to vaccine prioritisation, in order to simplify the rollout as much as possible, age was the primary driving force in determining the order of vaccine rollout. The other priority groups were largely based around shielding the elderly population (medical and social care workers).
By contrast, the US has adopted an approach whereby it was preferable to ramp up the overall percentage of people vaccinated, including offering vaccines to younger people. Whilst there has been a degree of age prioritisation, it has certainly not been as strict as that in the US.
On the face of it, this would mean that younger more tech-savvy individuals would be able to secure bookings ahead of older individuals. In the short term, this would increase the number of deaths given that COVID primarily discriminates upon age in fatalities.
However, this also causes a longer term problem too - it limits people's enthusiasm to get vaccinated. In behavioural psychology exclusivity is an important mechanism to getting people to choose a particular course of behaviour.
When older people are prioritised, they feel the vaccine is more exclusive and thus will be more likely to adopt it. Indeed, the UK is currently struggling to ramp up vaccine uptake amongst its youngest population with vaccinations now available to everyone.
The Government is even resorting to other behavioural science interventions targeted at this group, including incentives and threatening vaccine passports for nightclubs. Such measures are often more associated with the US and haven't been needed in the UK so far.
Lots of countries will be looking at England for insights into how COVID relaxation could play out elsewhere – but need to look beyond comparisons of overall % vaccinated nationally, because age distribution could mean very different outcomes in terms of severe disease. https://t.co/DsBOMLGgPh
— Adam Kucharski (@AdamJKucharski) August 16, 2021
Dosing Intervals
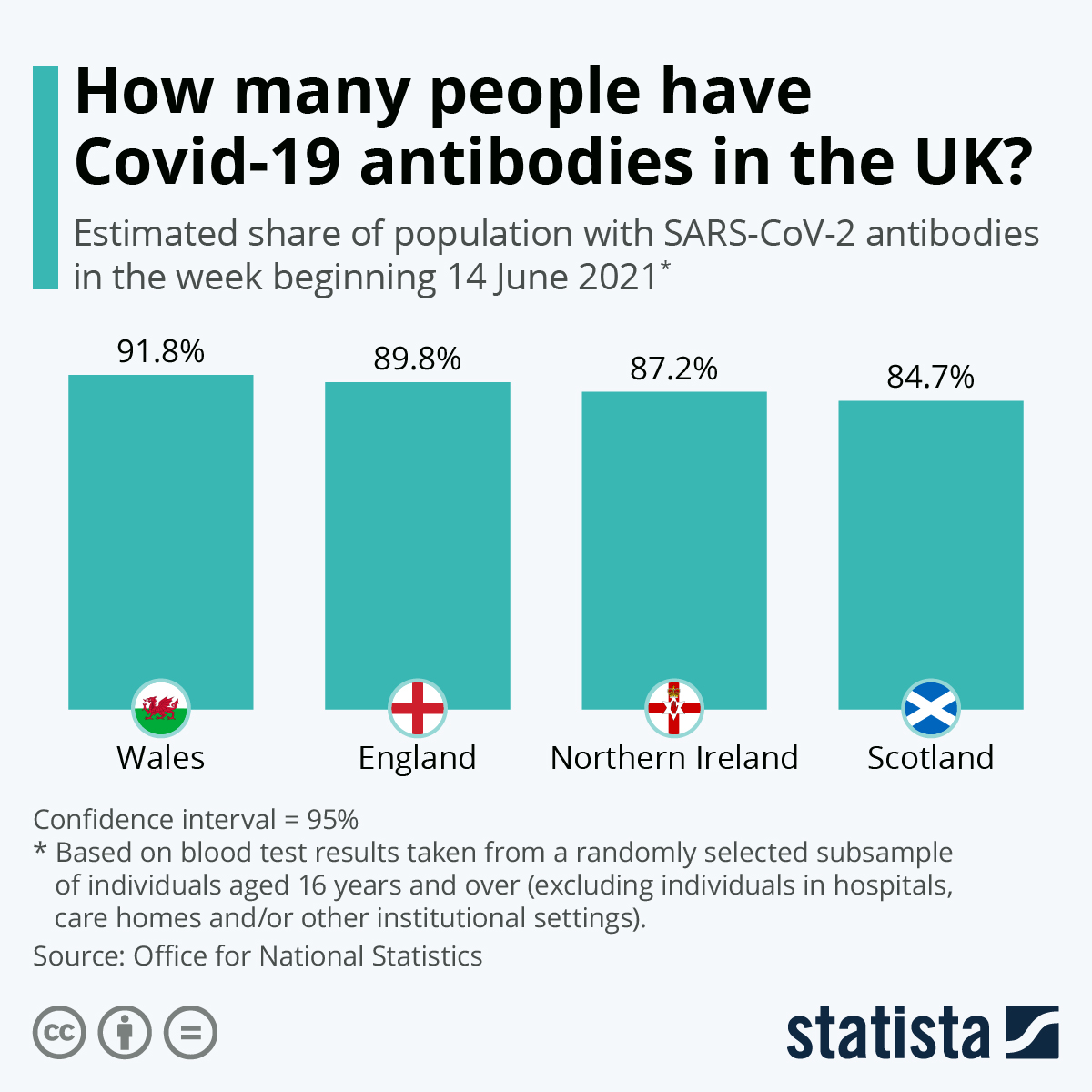
Not all vaccinations get the result you're after. A strong antibody response isn't guaranteed for all individuals who are vaccinated.
The UK made a decision early on during the rollout to use a 8-12 week dosing interval for vaccines to maximise the amount of people who got their first jab.
By contrast, the US has stuck to using a dosing interval of typically 3 weeks.
The evidence has mounted that a 12 week vaccine dose interval produces the best results, yet the US hasn't followed in adopting this approach:
- Delaying second Pfizer vaccines to 12 weeks significantly increases antibody responses in older people, finds study
- Timing of Booster Dose and Efficacy of ChAdOx1 nCoV-19 Vaccine
- Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials
Despite this evidence, the World Health Organisation also stuck to recommending a maximum of a 6 week interval of vaccine doses.
As a bonus, the UK's use of the Oxford/AstraZeneca vaccine (which creates a robust T-Cell response) ‘may protect against Covid for longer and eliminate need for booster’ - thus offering high levels of protection without people needing to come back for boosters (as is already planned for mRNA vaccines).
Incidentally, South Korea started mixing and matching doses of Pfizer and AstraZeneca. A recent study has found that having a first dose of AstraZeneca followed by a dose of Pfizer offers a superior immune response than vaccination with just one brand.
So this chart above measures the first dose after 28 days, and the second after 11-12 weeks hence the higher VE % for AstraZeneca! But this would make sense. Why? Because everyone knows AstraZeneca is a SLOW BURNER. It takes time to build up to a significant effect but it always pic.twitter.com/ElFgfDCcwC
— Chise 🧬🧫🦠💉 (@sailorrooscout) May 23, 2021
Paying for 'Expert' Decisions
Accountability matters. Decisions about whether societies face further deaths or lockdowns currently largely depends on the decisions of experts. These decisions affect people's willingness to be vaccinated and the effectiveness of the vaccines once when they receive them.
It is not sufficient anymore for Twitter experts to pass the blame to antivaxers - they must own the decisions that drive the results we see, particularly during COVID vaccination programs.
Instead of gaming the numbers for the percentage of the population vaccinated, it is vital instead to consider the percentage of the population who have been effectively vaccinated.